Retinal eye cells grown in the lab show potential for treating blindness through successful connections, paving the way for clinical trials.
“My eyes reveal what my tongue could never express.” Eyes are more than an organ to us humans, they open the world to us and us to the world. Scientists have long been working to find solutions to enhance the vision of our eyes, repair our eyes and cure blindness.
Science has made progress and many conditions that can lead to reduced or loss of vision can be treated. But, there is a hurdle that needs to be overcome, eyes as an organ can be replenished but what about the vision?
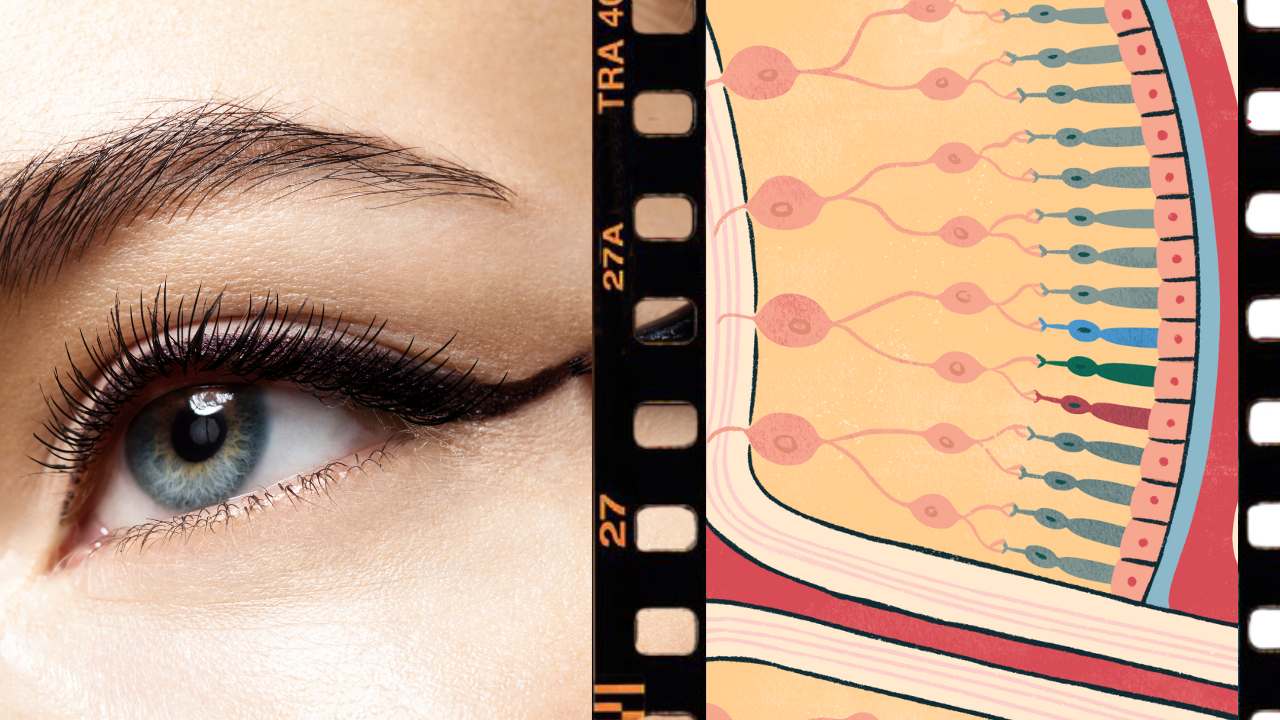
Eyes can be compared to a camera where the glasses can be fixed but what about the image on the sensor? Our brain is like a sensor that interprets the light falling on the lens and creates imagery. These electrical signal-like impulses are carried out by an intricate network of neurons which are the nerve cells.
Once there is a hindrance in this intricate network of neurons that travel through our nerves it becomes difficult to reverse the impact.
The good news, a recent study found that cells grown in a lab from stem cells, called retinal cells, are able to connect with other cells around them, which is an important step in treating eye disorders.
Researchers from the University of Wisconsin-Madison have been working on growing clusters of cells called organoids that are similar to the retina, the part of the eye that helps us see.
They take skin cells and change them into stem cells and then make them turn into different types of retinal cells, which help us see and send that information to the brain.
This new discovery about the ability of lab-grown cells to connect with other cells could mean that these cells are ready for use in treatments for humans with eye problems.
“We wanted to use the cells from those organoids as replacement parts for the same types of cells that have been lost in the course of retinal diseases,” says David Gamm, the UW–Madison ophthalmology professor and director of the McPherson Eye Research Institute whose lab developed the organoids.
“But after being grown in a laboratory dish for months as compact clusters, the question remained — will the cells behave appropriately after we tease them apart? Because that is key to introducing them into a patient’s eye.”
During 2022, Gamm and UW–Madison collaborators published studies demonstrating that dish-grown retinal cells called photoreceptors respond like those in a healthy retina to different wavelengths and intensities of light and that once they are separated from adjacent cells in their organoid, they can reach out toward new neighbors with characteristic biological cords called axons.
“The last piece of the puzzle was to witness if these cords had the capacity to plug into, or shake hands with, other retinal cell types in order to communicate,” says Gamm, whose new results on successful connections between the cells were published today in the Proceedings of the National Academy of Sciences.
Cells in the retina and brain communicate across synapses, tiny gaps at the tips of their cords.
To confirm that their lab-grown retinal cells have the capacity to replace diseased cells and carry sensory information like healthy ones, the researchers needed to show that they could make synapses.
Xinyu Zhao, UW–Madison professor of neuroscience and co-author of the new study, worked with the Gamm lab’s cells to help study their ability to form synaptic connections.
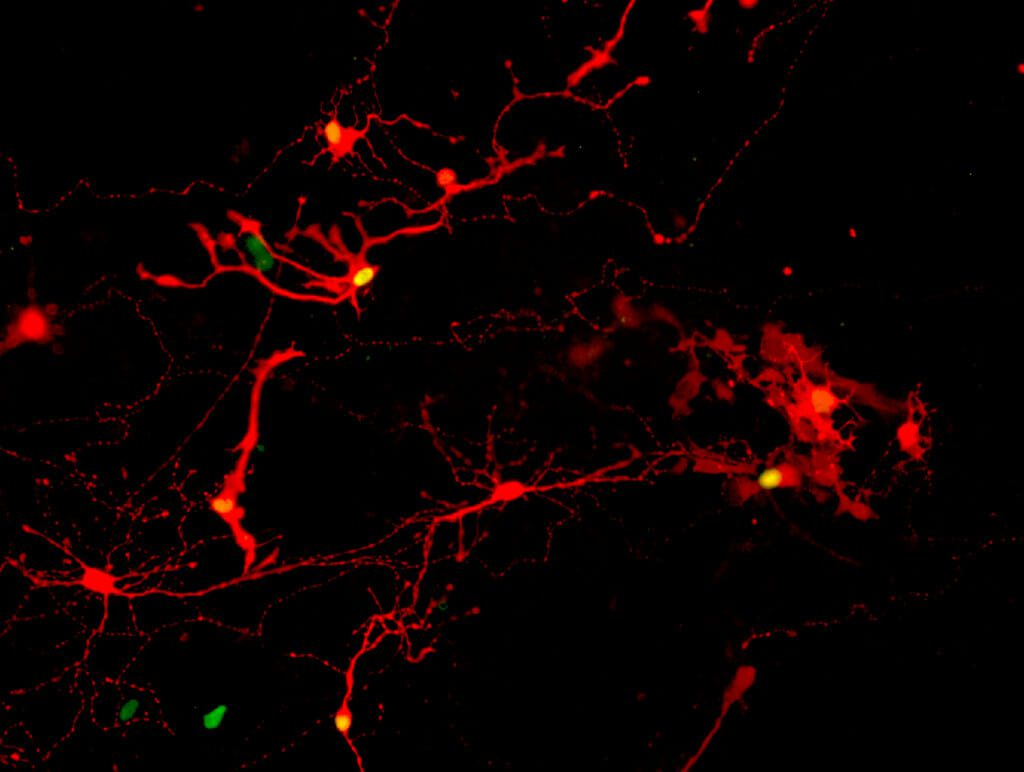
They did this using a modified rabies virus to identify pairs of cells that could form the means to communicate with one another.
The research team, including graduate students and co-first-authors Allison Ludwig and Steven Mayerl, broke apart the retinal organoids into individual cells, gave them a week to extend their axons and make new connections, exposed them to the virus, and then took a peek.
What they saw were many retinal cells marked by a fluorescent color indicating a rabies infection had infected one across a synapse successfully formed between neighbors.
“We’ve been quilting this story together in the lab, one piece at a time, to build confidence that we’re headed in the right direction,” says Gamm, who patented the organoids and co-founded Madison-based Opsis Therapeutics, which is adapting the technology to treat human eye disorders based on the UW–Madison discoveries.
“It’s all leading, ultimately, to human clinical trials, which are the clear next step.”
After they confirmed the presence of synaptic connections, the researchers analyzed the cells involved and found that the most common retinal cell types forming synapses were photoreceptors – rods and cones – which are lost in diseases like retinitis pigmentosa and age-related macular degeneration, as well as in certain eye injuries.
The next most common cell type, retinal ganglion cells, are degenerate in optic nerve disorders like glaucoma.
“That was an important revelation for us,” says Gamm. “It really shows the potentially broad impact these retinal organoids could have.”