The communication was clear, “We have a simple message to all countries – test, test, test,” the advice of the World Health Organisation (WHO) head Tedros Adhanom Ghebreyesus had for the world to contain the deadly pandemic.
South Korea followed the same approach and isolated infected people based on widespread testing. The strategy was successful and admired across the world. It even managed to hold an election during the pandemic, thanks to the massive testing drive it adopted as a strategy to fight the COVID-19 outbreak.
Now, bring in a country with almost 25 times the population of South Korea– Like many nations, India did not have enough kits to test most of its population for the new coronavirus.
India’s strategy to deal with COVID-19 pandemic

India has instead relied on people’s power and proactive social distancing through strict lockdown. The first phase of lockdown was started on March 25 and ended on April 14. India is in its second phase of lockdown that will last till May 3.
Undoubtedly, India has introduced some of the most stringent measures in the world to contain the virus. The analysis of the data represents a mixed result, more on that later.
The personal appeal of Prime Minister Modi and comparatively widespread support for his initiative seemed to work in the early stages of the lockdown.
Furthermore, thousands of health-care workers are continuously fanning out across the country to trace and quarantine people who might have had contact with those with COVID-19. People are generally only tested if they develop symptoms.
India has also started testing random samples from across the country to assess the spread. The results help it track if the disease is spreading in communities. Some states are planning to do a door-to-door screening in hot zones, Bihar has already initiated the process.
The weeks and months ahead will show whether these steps have been enough. It still can’t be determined whether India has escaped community transmission.
The only way to know will be to conduct a massive testing drive. Later a mass level antibody testing will also shed light on percentage of the population infected. Moreover, if and when there is an explosion of infections and more sick people require hospitalization, India will face tremendous challenges.
India with a population of 1.3 billion, does intend to preempt such a situation from developing. Its fragile healthcare infrastructure will not be able to cope with such an outbreak.
Every Indian state today has similar priorities– add new beds, increase the capacity of intensive care units (ICUs), requisition portions of private hospitals, increase the number of lifesaving ventilators, recruit medical practitioners on contract, decide on extending services of retiring doctors and nurses and earmark select government hospitals for COVID-19 patients.
The blueprint also encompasses converting medical colleges and railway coaches into isolation wards, stadiums into quarantine facilities, and readying part of hospitals under defense, central police forces, and railways for COVID-19 patients.
In India, as in most nations, not all available ventilators can be plugged out from the intensive care units. So, the number of equipment that can be made available for COVID-19 interventions is far too less considering the large population of India.
With almost all countries in the world fighting their own battle to contain the virus in their respective countries, India will have to rely majorly on domestic industries to prop up the supply. To be honest, it will never be sufficient if India can’t stop the numbers to explode. At the moment with extension lockdown to 19 more days, things look under control.
The Indian approach is not without its flaws

Testing still needs to be an essential part of India’s COVID-19 control strategy and expanded rapidly, or infections will be missed, says Gagandeep Kang, executive director of the Translational Health Science and Technology Institute in Faridabad.
Some people with the virus don’t have symptoms, so their infections won’t be detected unless they’re tested. “There is going to be no solution to this without testing,” says Kang.
According to ICMR, 244,893 samples from 229,426 individuals have been tested as of 14 April — one of the lowest test rates per capita in the world.
Various states in India also have large variations in the number of tests done. It essentially means that for some states in India, with a population comparable to a country, the testing is way behind.
Flattening the curve
The “curve” you may have heard about and the researcher are talking about refers to the projected number of people who will contract COVID-19 over a period of time. (This is not a hard prediction of how many people will definitely be infected, but a theoretical number that’s used to model the virus’ spread.) Here’s how it looks like:
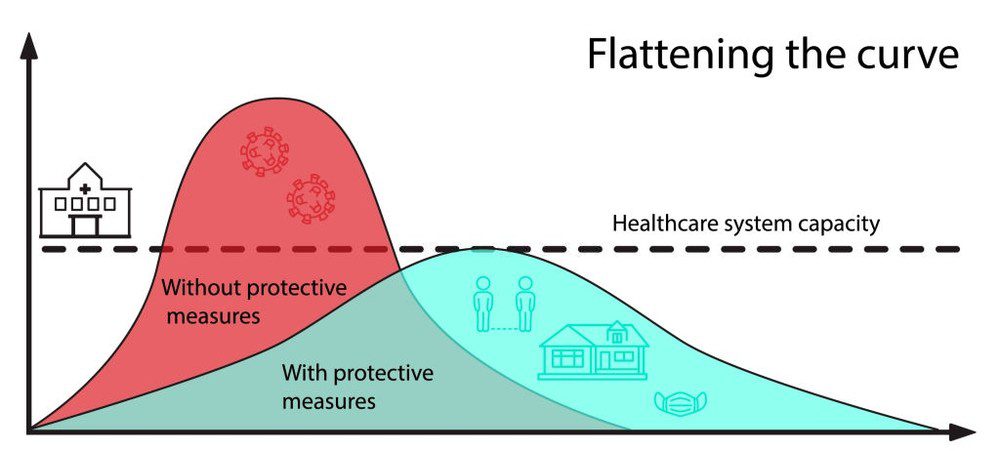
The curve takes on different shapes, depending on the virus’s infection rate. It could be a steep curve, in which the virus spreads exponentially (that is, case counts keep doubling at a consistent rate), and the total number of cases jumps to its peak within a few weeks.
Infection curves with a steep rise also have a steep fall– after the virus infects pretty much everyone who can be infected, case numbers begin to drop exponentially, too.
The faster the infection curve rises, the quicker the local health care system gets overloaded beyond its maximum capacity to treat people. As it has already been seen in Italy and Spain, more and more new patients may be forced to go without ICU beds, and more and more hospitals may run out of the basic supplies they need to respond to the outbreak.
This scenario becomes extremely perilous as there could be widespread deaths due to the non-availability of healthcare infrastructure due to other health problems. The fatality-rate in absence of critical medical care may also rise.
A flatter curve, on the other hand, assumes the same number of people ultimately get infected, but over a longer period of time. A slower infection rate means a less stressed healthcare system, fewer hospital visits and the need for critical care on any given day and fewer sick people being turned away.
India essentially is trying to flatten the curve through its lockdown measures. The problem remains that without massive testing and containment measures India may not be able to keep the infection rate within its healthcare capacity.
One other aspect that India has to look into will be to also increase the healthcare capacity to accommodate a higher infection rate. A series of guidelines to ease lockdowns from 20th April may be aimed towards getting more essential economic activity to achieve that.
Is lockdown working for India?
An external affairs ministry official claimed on April 9 that in the absence of a lockdown, there would have been 820,000 cases by April 15, according to an internal assessment. The actual number stood at little over 12,000 cases as on 15th April.
When asked about details of the internal assessment, the Indian Council of Medical Research (ICMR) initially said no such study existed and later clarified that the claim was made based on a “statistical extrapolation” by the ministry of health as depicted below
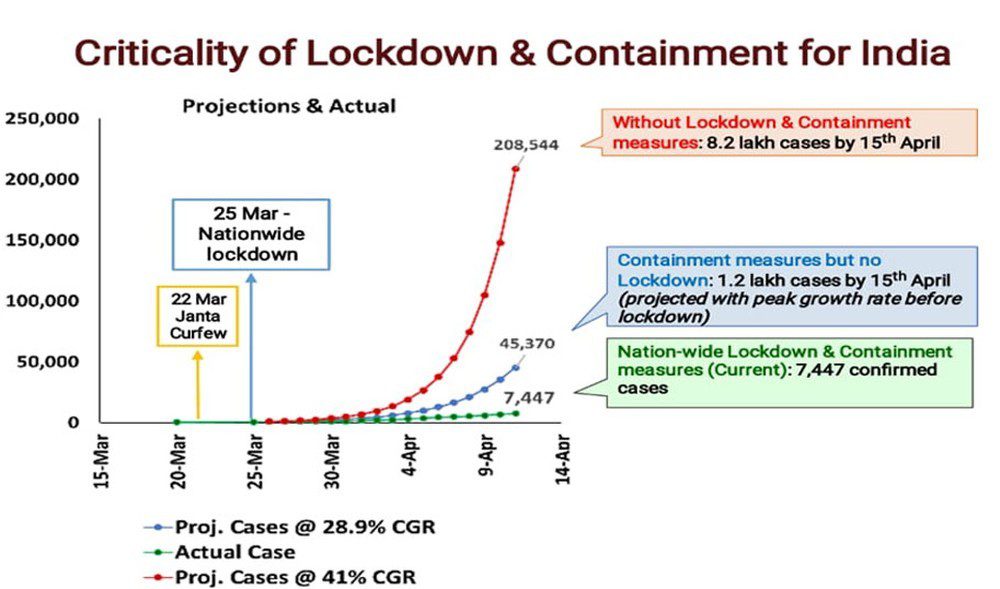
Going simply by the data given by external affairs ministry official the lockdown seems to have worked well for India. However, there are some grey areas.
One of the major challenges with the following data is that there is no clarification on what model was used to arrive at these numbers.
The model hasn’t been made public or even talked about by government officials. As it happens, the only model that ICMR has shared publicly is not about the lockdown, but an analysis of the border screening measures India introduced relatively earlier than other countries.
So what is the right way to asses if the first lockdown helped in slowing the infection and flatten the curve for India?
Without an official reference model in India, another approach remaining is to go on is aggregate data on total confirmed cases nationwide, which is updated every day. The chart below plots the natural logarithm of total cases on the vertical axis with the time index on the horizontal.
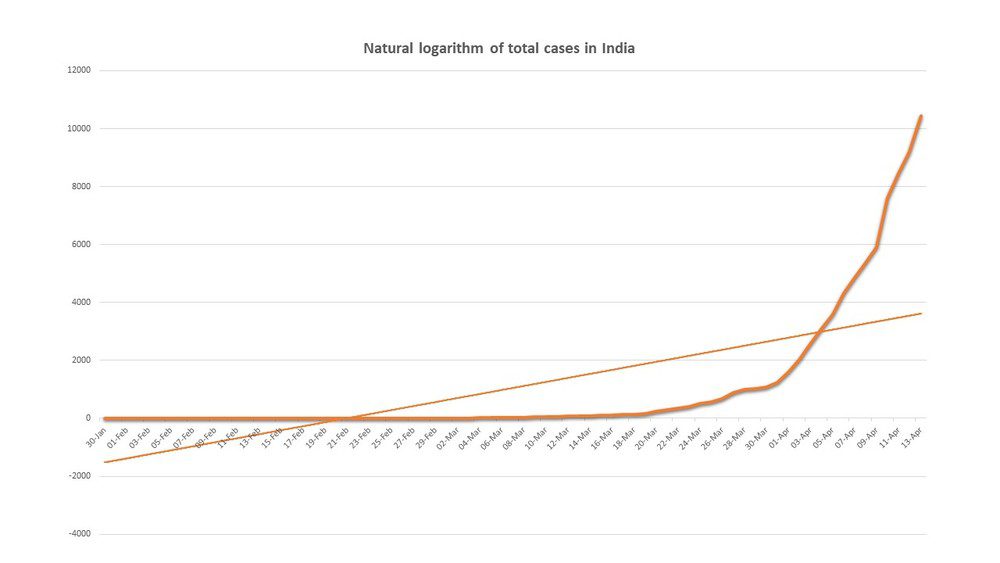
The interpretation is simple, the curve under the straight-line represents slowing in the rate of the infection and if the curve rises above the straight line, then infections are growing at a proportional rate. In other words, the classic exponential curve used in epidemiology.
It shows that after a basically flat portion with low growth in new cases, India entered the exponential phase, beginning March 16 or so. It’s worth noting that the curve starts to rise days before the first lockdown and continued to grow till the point it rose above the straight line around April 3.
A real optimist may interpret a small flattening of the curve from around March 30, but this is just only a few days after the lockdown. Given that the virus has a 14 days incubation period, it obviously cannot be attributed to the lockdown.
What is more, several states had initiated their own lockdowns in advance of the national one. Karnataka, for instance, announced one on March 13, Maharashtra on March 20.
If the lockdown had a major effect, you would expect the slope of this line to flatten or bend toward the horizontal axis. This doesn’t mean to say that lockdown did not have any effect. Maybe the infection rate growth could have been even higher without it.
But, there is a huge economic cost to the two lockdowns that India will have to bear at least in the short to middle term. Considering the overall scenario the first lockdown is at best given a mixed result for India. The results of the second lockdown will be analyzed further to reach a conclusion.
The brighter side of India’s handling of COVID-19 epidemic

In many ways, it is all about India trying to battle a pandemic with limited resources. Experts talk about the country’s success in defeating polio, combating smallpox, successfully controlling the spread of HIV/Aids, and more recently H1N1 with rigorous surveillance, sharp identification of vulnerable people, targeted intervention, and early engagement with the private sector to prevent disease spread.
Still, epidemiologists say that India’s strategy to trace and quarantine contacts, along with the government’s decision to order the country’s roughly 1.3 billion inhabitants to stay at home for 21 days from late March, have probably helped to slow the spread of the virus in some places.
A further extension of 19 days in lockdown has definitely bought the country time to prepare its ailing health-care system. Under the lockdown, people are allowed out for essentials, such as food and medical care, but in most states, people under quarantine are closely monitored by social workers and cannot leave their homes in some places.
The stakes are high– if the current containment measures fail to slow viral spread, experts say, further restrictions to keep people apart will be needed. Any further extension of the lockdown would be very hard on people who need to work to feed themselves. A timely, yet massive testing may be the way out for India.