There has been a lot of talks recently about the new coronavirus variant. The fast spread of the new variant of coronavirus has been blamed for the strict tier four mixing rules for millions of people, harder restrictions on mixing at Christmas in England, Scotland, and Wales, while other countries including India are restricting travel from the UK.
The new strain was first discovered by Public Health England’s genomic surveillance, and it cautioned the Boris Johnson govt about its seriousness on 18 December.
The now infamous new strain, named VUI-202012/01 (first variant under investigation in December 2020), is said to be nearly 70 percent more infectious and Health Secretary Matt Hancock said Sunday that it “was out of control”.
Outside of the UK, the new variant has already been identified in Denmark, Italy, the Netherlands and Australia. However, it is not believed to be as widespread as the UK.
Why is this new coronavirus variant causing alarm?
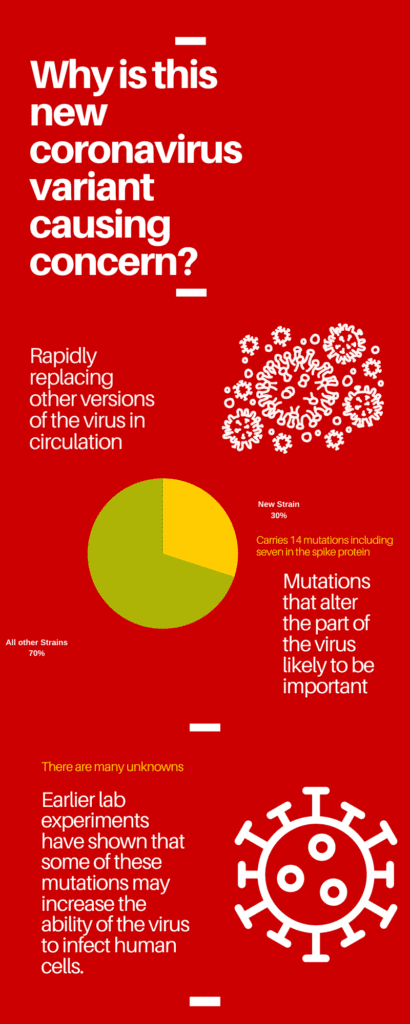
Three major things, all at one time is what is raising some concerns:
- It is quickly replacing other variants of the virus in circulation
- It has marked mutations that alter the part of the virus likely to be important — spike protein
- Earlier lab experiments have shown that some of these mutations may increase the ability of the virus to infect human cells.
The variant carries 14 defining mutations including seven in the spike protein, the protein that mediates entry of the virus into human cells. This is a relatively large number of changes compared to the many variants we have in circulation globally.
All of these come together to build a case for a virus that can spread more easily.
However, this can’t be conclusively established as of now. New strains can become more common simply by being in the right place at the right time – such as London, which had a lower level of restrictions until recently.
But already the justification for tier four restrictions is in part to reduce the spread of the variant.
“Laboratory experiments are required, but do you want to wait for weeks or months [to see the results and take action to limit the spread]? Probably not in these circumstances,” Prof Nick Loman, from the Covid-19 Genomics UK Consortium, told BBC.
[rb_related title=”You May Also Like” total=”2″ ids=”7949,7893″]
How much faster has it spread?
It was first detected in September. In November around a quarter of cases in London were the new variant. This reached nearly two-thirds of cases in mid-December.
You can see how the variant has come to dominate the results of testing in some centers such as the Milton Keynes Lighthouse Laboratory.
Mathematicians have been running the numbers on the spread of different variants in an attempt to calculate how much of an edge this one might have.
It’s not easy to attribute how much is due to people’s behavior and what is due to the virus. The figure mentioned by the UK Prime Minister Boris Johnson was that the variant may be up to 70% more transmissible.
He said this may be increasing the R number – which indicates if an epidemic is growing or contracting – by 0.4. That 70% number appeared in a presentation by Dr. Erik Volz, from Imperial College London, on Friday.
During the talk, he said: “It is really too early to tell… but from what we see so far it is growing very quickly, it is growing faster than (a previous variant) ever grew, but it is important to keep an eye on this.” There is no “nailed on” figure for how much more infectious the variant may be.
The most important question still remains if the new strain is more infectious or not. Followed by the severity of the infection that it causes.
“The amount of evidence in the public domain is woefully inadequate to draw strong or firm opinions on whether the virus has truly increased transmission,” said Prof Jonathan Ball, a virologist at the University of Nottingham.
How far has it spread?
It is thought the variant either emerged in a patient in the UK or has been imported from a country with a lower ability to monitor coronavirus mutations.
The variant can be found across the UK, except Northern Ireland, but it is heavily concentrated in London, the South East and eastern England. Cases elsewhere in the country do not seem to have taken off.
Data from Nextstrain, which has been monitoring the genetic codes of the viral samples around the world, suggest cases in Denmark and Australia have come from the UK. The Netherlands has also reported cases.
A similar variant that has emerged in South Africa shares some of the same mutations, but appears to be unrelated to this one.
Has this happened before?
Yes. The virus that was first detected in Wuhan, China, is not the same one you will find in most corners of the world.
How many times has the Sars-CoV-2 virus mutated?
So far, scientists have noted two major distinct set of mutations in the virus that causes Covid-19, the H69/V70 deletion, and the D614G, both of which affects the spike proteins, which helps the virus to bind to the human cell and infect it.
It is this ability that vaccines seek to target and weaken. The H69-70 deletion affects antibody susceptibility and has been seen three times so far- in Danish minks, in Britain, and in a patient who was rendered much less responsive to convalescent plasma therapy.
The virus was first reported in Wuhan and since then, it is said to have mutated many times, most of which have gone unnoticed. The BBC reported that if the strain that’s infecting people now is compared to the first one that spread in Wuhan a total of 25 mutations will be visible, that’s a little over two mutations a month. As the human body gets more adept at identifying and fighting it, the virus too is expected to fight back, by trying to evade the body’s immune system.
The D614G is the first known mutation that is suspected to have occurred in Eastern China in January and later spread through New York City and Europe. Within a few months of the pandemic, this particular variant was found all over the world, as it had successfully replaced its predecessor, which had spread from Wuhan.
What do we know about the new mutations?
An initial analysis of the new variant has been published and identifies 17 potentially important alterations.
There have been changes to the spike protein – this is the key the virus uses to unlock the doorway to our body’s cells.
One mutation called N501Y alters the most important part of the spike, known as the “receptor-binding domain”.
This is where the spike makes first contact with the surface of our body’s cells. Any changes that make it easier for the virus to get inside are likely to give it an edge.
“It looks and smells like an important adaptation,” said Prof Loman.
The other mutation – a H69/V70 deletion, in which a small part of the spike is removed – has emerged several times before, including famously in infected mink.
Work by Prof Ravi Gupta at the University of Cambridge has suggested this mutation increases infectivity two-fold in lab experiments.
Studies by the same group suggest the deletion makes antibodies from the blood of survivors less effective at attacking the virus.
Prof Gupta told me: “It is rapidly increasing, that’s what’s worried government, we are worried, most scientists are worried.”
Where has it come from?
Backward tracing using genetic evidence hints that the new UK variant emerged in September and then circulated at very low levels in the population until mid-November, according to Public Health England (PHE).
“The increase in cases linked to the new variant first came to light in late November when PHE was investigating why infection rates in Kent were not falling despite national restrictions.
We then discovered a cluster linked to this variant spreading rapidly into London and Essex,” the agency said. Multiple experts have suggested that this new variant could have been amplified because of a superspreader event; it could be the mutation somehow makes it spread more easily without causing more serious illness, or it could have been by chance.
Moreover, it is well known that the variant is unusually highly mutated.
The most reasonable explanation is the variant has appeared in a patient with a weakened immune system that was unable to beat the virus.
Instead, their body became a breeding ground for the virus to mutate.
Is the new coronavirus strain more deadly?
At the moment there is no evidence to suggest that it does, although this will need to be carefully watched. Only lab tests can confirm whether it is the case.
However, a rapid transmission that is most feared for this new strain would be enough to cause problems for hospitals.
If the new variant signifies that more people are infected more swiftly, that would, in turn, lead to more people needing hospital treatment and quickly overwhelm the healthcare infrastructure.
Will the vaccines work against the new variant?
Almost certainly yes, based on the information at of now.
All three leading vaccines develop an immune response against the existing spike, which is why the question comes up.
Vaccines train the immune system to attack many different parts of the virus, so even though part of the spike has mutated, the vaccines should still work.
“But if we let it add more mutations, then you start worrying,” said Prof Gupta.
“This virus is potentially on a pathway for vaccine escape, it has taken the first couple of steps towards that.”
Vaccine escape happens when the virus changes so it evades the full effect of the vaccine and proceeds to infect people.
This may be the most disturbing aspect of the new mutation.
This variant is just the latest to show the virus is continuing to adapt as it infects more and more of us.
A presentation by Prof David Robertson, from the University of Glasgow on Friday, concluded: “The virus will probably be able to generate vaccine escape mutants.”
That would put us in a situation similar to flu, where the vaccines need to be regularly updated. Luckily, the vaccines we have are very easy to tweak.